22q11.2 Deletion Syndrome: Symptoms, Causes, Diagnosis, Treatment
 |
| Justin Gigliotti’s Tweet. |
#HeyJustin Trends as Man With 22q11.2 Deletion Syndrome Asks for Millions of Hellos
The AMassachusetts-based content creator and activist was the focus of a Twitter trending topic on Monday. The trend was in relation to a video he released raising awareness of his syndrome while calling on users of the site to say hello and share his hashtag, Newsweek reported.
Boston resident Justin Gigliotti, who uses the handle @syndrome22q1, received a wave of support from users of the social network after uploading the short 29-second clip to his profile that was seeking "hellos from millions of people from around the world."
The term #HeyJustin became a trending topic and had been used over 18,000 times as of Tuesday morning. His tweet attracted over 13,000 responses.
Gigliotti explained in the video upload that he had a disability called 22q syndrome and he was "curious" to see how many people would respond to his request. He added: It would make my day... it would make my heart happy, it would make me happy."
Gigliotti, who is also known on his accounts as Justin G, has repeatedly used the profile for similar social campaigns over the past month, promoting hashtags centered around his name and tagging profiles to signal-boost his account and raise awareness.
 |
| Justin Gigliotti is a 22q patient (Justin G/Twitter) |
Donald Trump's estranged niece Mary L Trump shared the video with the hashtag #HeyJustin.
"#HeyJustin keep making the world a better place, Buddy!" wrote Michael Zapcic, while Paula Poundstone wrote, "#HeyJustin I hope you're doing okay during the pandemic. Stay strong, Sir."
"Meet Monica my Granddaughter, age 7, Non-Verbal Autism, Severe Sensory Processing Who loves Star Wars, Pop Music, Roller Skating, and The Voice! #HeyJustin," said a user. "Hey, Justin! My brother Mark also has a disability (Down syndrome) and he says hello! #HeyJustin" tweeted another.
People also share adorable photos of their pets to give a shoutout to Justin. One user wrote: "#HeyJustin Hope you're having an amazing day and my cat cucumber says hi as well." Another wrote, "#HeyJustin coming from the Okanagan in British Columbia. These are my dogs, Dugg and Ollie."
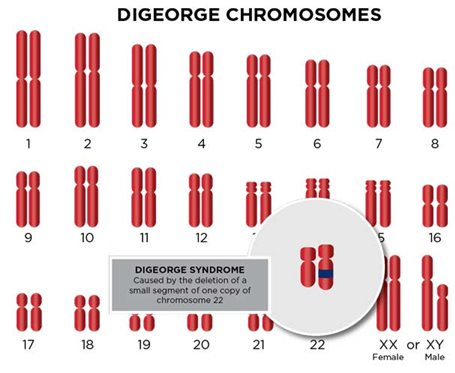
DiGeorge syndrome: Overview
DiGeorge syndrome, more accurately known by a broader term — 22q11.2 deletion syndrome — is a disorder caused when a small part of chromosome 22 is missing. This deletion results in the poor development of several body systems, according to Mayoclinic.
The term 22q11.2 deletion syndrome covers terms once thought to be separate conditions, including DiGeorge syndrome, velocardiofacial syndrome, and other disorders that have the same genetic cause, though features may vary slightly.
Medical problems commonly associated with 22q11.2 deletion syndrome include heart defects, poor immune system function, a cleft palate, complications related to low levels of calcium in the blood, and delayed development with behavioral and emotional problems.
The number and severity of symptoms associated with 22q11.2 deletion syndrome vary. However, almost everyone with this syndrome needs treatment from specialists in a variety of fields.
DiGeorge syndrome: Symptoms
Signs and symptoms of DiGeorge syndrome (22q11.2 deletion syndrome) can vary in type and severity, depending on what body systems are affected and how severe the defects are. Some signs and symptoms may be apparent at birth, but others may not appear until later in infancy or early childhood.
Signs and symptoms may include some combination of the following:
- Heart murmur and bluish skin due to poor circulation of oxygen-rich blood (cyanosis) as a result of a heart defect
- Frequent infections
- Certain facial features, such as an underdeveloped chin, low-set ears, wide-set eyes, or a narrow groove in the upper lip
- A gap in the roof of the mouth (cleft palate) or other problems with the palate
- Delayed growth
- Difficulty feeding, failure to gain weight, or gastrointestinal problems
- Breathing problems
- Poor muscle tone
- Delayed development, such as delays in rolling over, sitting up, or other infant milestones
- Delayed speech development or nasal-sounding speech
- Learning delays or disabilities
- Behavior problems
DiGeorge syndrome: Causes
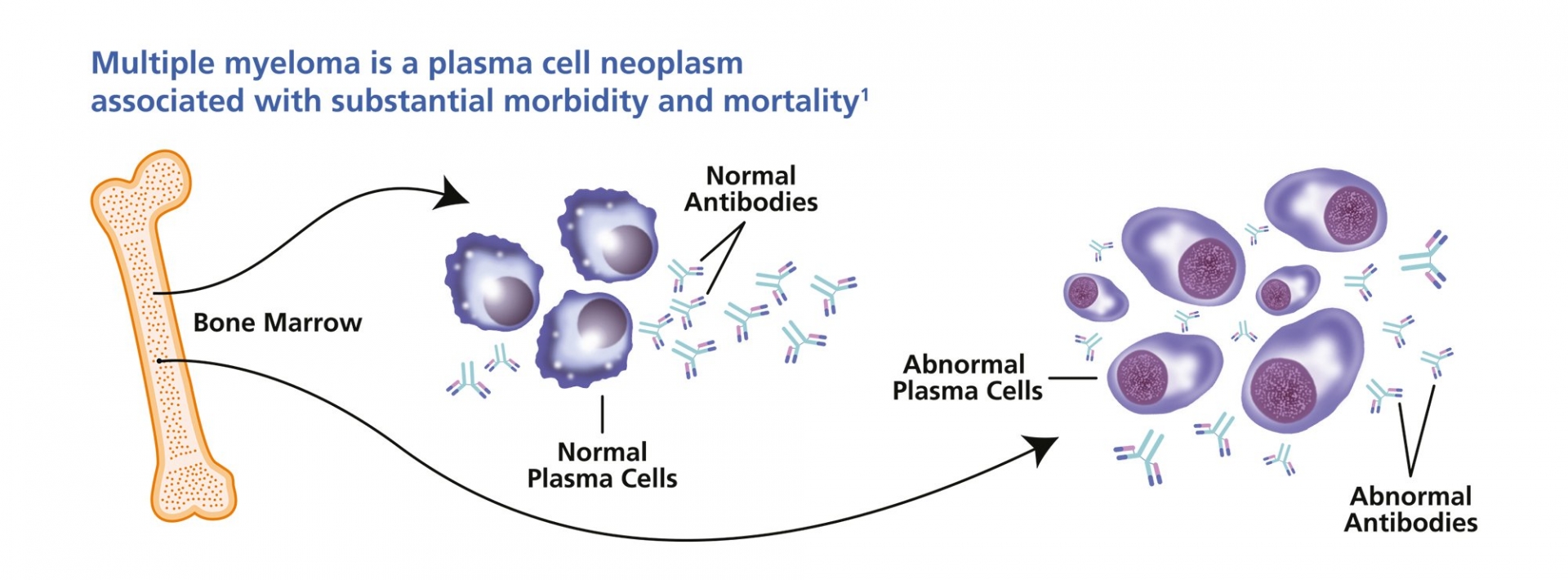
Each person has two copies of chromosome 22, one inherited from each parent. If a person has DiGeorge syndrome (22q11.2 deletion syndrome), one copy of chromosome 22 is missing a segment that includes an estimated 30 to 40 genes. Many of these genes haven't been clearly identified and aren't well-understood. The region of chromosome 22 that's deleted is known as 22q11.2.
The deletion of genes from chromosome 22 usually occurs as a random event in the father's sperm or in the mother's egg, or it may occur early during fetal development. Rarely, the deletion is an inherited condition passed to a child from a parent who also has deletions in chromosome 22 but may or may not have symptoms.
 |
| KidStock / Getty Images |
DiGeorge syndrome: Complications
The portions of chromosome 22 deleted in DiGeorge syndrome (22q11.2 deletion syndrome) play a role in the development of a number of body systems. As a result, the disorder can cause several errors during fetal development. Common problems that occur with 22q11.2 deletion syndrome include:
- Heart defects. 22q11.2 deletion syndrome often causes heart defects that could result in an insufficient supply of oxygen-rich blood. For example, defects may include a hole between the lower chambers of the heart (ventricular septal defect); only one large vessel, rather than two vessels, leading out of the heart (truncus arteriosus); or a combination of four abnormal heart structures (tetralogy of Fallot).
- Hypoparathyroidism. The four parathyroid glands in the neck regulate the levels of calcium and phosphorus in the body. 22q11.2 deletion syndrome can cause smaller than normal parathyroid glands that secrete too little parathyroid hormone (PTH), leading to hypoparathyroidism. This condition results in low levels of calcium and high levels of phosphorus in the blood.
- Thymus gland dysfunction. The thymus gland, located beneath the breastbone, is where T cells — a type of white blood cell — mature. Mature T cells are needed to help fight infections. In children with 22q11.2 deletion syndrome, the thymus gland may be small or missing, resulting in poor immune function and frequent, severe infections.
- Cleft palate. A common condition of 22q11.2 deletion syndrome is a cleft palate — an opening (cleft) in the roof of the mouth (palate) — with or without a cleft lip. Other, less visible abnormalities of the palate that may also be present can make it difficult to swallow or produce certain sounds in speech.
- Distinct facial features. A number of particular facial features may be present in some people with 22q11.2 deletion syndrome. These may include small, low-set ears, short width of eye openings (palpebral fissures), hooded eyes, a relatively long face, an enlarged nose tip (bulbous), or a short or flattened groove in the upper lip.
- Learning, behavioral, and mental health problems. 22q11.2 deletion may cause problems with the development and function of the brain, resulting in learning, social, developmental, or behavioral problems. Delays in toddler speech development and learning difficulties are common. Some children develop attention-deficit/hyperactivity disorder (ADHD) or autism spectrum disorder. Later in life, the risk of depression, anxiety disorders, and other mental health disorders increases.
- Autoimmune disorders. People who had poor immune function as children, due to a small or missing thymus, may also have an increased risk of autoimmune disorders, such as rheumatoid arthritis or Graves' disease.
- Other problems. A large number of medical conditions may be associated with 22q11.2 deletion syndrome, such as hearing impairment, poor vision, breathing problems, poor kidney function, and relatively short stature for one's family.
DiGeorge syndrome: Diagnosis
DiGeorge syndrome is typically diagnosed at birth or soon after birth based on the signs and symptoms of the disorder. Genetic testing can then be performed to confirm deletions on chromosome 22.
In some children, all of the classical features of DiGeorge syndrome will be seen at birth. In others, the presentation may be subtle and only be recognized when an impairment, either physical or development, become apparent.
Due to the variability of symptoms, genetic testing must be performed to confirm the diagnosis. This can be tricky since the pattern of deletions can often be so different, even between family members. The most reliable forms of genetic testing include:
- Fluorescence in situ hybridization (FISH), in which a fluorescent agent binds to a chromosome to help identify its genetic sequence.
- Quantitative polymerase chain reaction (qPCR), which amplifies the number of chromosomes and evaluates their sequence using radioactive binding agents.
- Multiplex ligation-dependent probe amplification assay (MLPA), a newer variation of the PCR.
The tests look at a specific portion of chromosome 22 called position 22q11.2. They only require a blood sample and are 95% accurate. Test results are usually returned within three to 14 days.
Other tests can be used for prenatal or postnatal screening, including array comparative genomic hybridization (array-CGH), a test that can scan the entire genome of fetal cells and deliver results within five days.
 |
| Photo: Ssmhealth |
DiGeorge syndrome: Treatment
There is no cure for DiGeorge syndrome. However, there are treatments available to address the various aspects of the disorder. The key is to identify and address each symptom under the care of a coordinating physician.
The care team may include specialists in maternal and fetal medicine, pediatrics, cardiothoracic surgery, learning disabilities, endocrinology, immunology, speech pathology, and audiology. A geneticist and genetic counselor are key members of the team.
Depending on the symptomatic presentation of the disease, various treatments may be prescribed for the following conditions:
- Heart defects are most often treated with surgery soon after birth to repair the heart and correct blood circulation problems.14
- Cleft palates can usually be surgically repaired.
- Parathyroid problems are typically treated with lifelong calcium and vitamin D supplements to correct nutritional deficiencies.15
- Mild thymus dysfunction can be usually be addressed by vaccinating children against the plethora of diseases that their immune systems will be able to fight. Antibiotics are often typically prescribed.
- Severe thymus dysfunction, in which the impairment is severe or the thymus gland is completely missing, may require a thymus or bone marrow transplant.16
- Child development problems require a multidisciplinary approach, often including speech therapy, special education, occupational therapy, and developmental therapy.
- Mental health issues may require therapy and pharmaceutical drugs to manage conditions like ADHD, depression, autism spectrum disorders, and schizophrenia.
The outlook of treatment can vary by the severity of the symptoms; there is not a single disease pathway or expected outcome.
However, many of the characteristic symptoms tend to resolve or become manageable over time with appropriate treatment. Others, particularly mental health issues, may develop and worsen over time—particularly those involving psychosis and schizophrenia. Early identification and intervention can greatly reduce the impact of these conditions.
Unlike some chromosomal deletion disorders, DiGeorge syndrome is not inherently associated with a shortened life span. Many people can live long, healthy lives and even have children.
DiGeorge syndrome: Prevention
DiGeorge syndrome is a heterozygous chromosomal disorder, meaning that it is caused by the deletion of genes missing only one of the two copies of chromosome 22. There is no known case of both copies being affected (a condition referred to as homozygosity), said Verywellhealth.
The only way to prevent DiGeorge syndrome is by preventing the passing on of the chromosomal mutation to a baby.
Given that only around 10% of cases are directly associated with familial inheritance, this is more difficult than it seems.10
As such, efforts are less focused on primary prevention (preventing disease before it occurs) and more on secondary prevention (preempting symptoms and complications once a disease is diagnosed). To this end, genetic testing is recommended for parents whose child has been positively diagnosed with DiGeorge syndrome.18
Overall, more severe cardiac, parathyroid, and thymus-related diseases are seen in children for whom a relative has a 22q11.2 deletion.
DiGeorge syndrome: Coping
Having a child with DiGeorge syndrome can be challenging. As a parent, you may need to manage multiple treatment issues with multiple providers while addressing the special needs of your child. Moreover, you would need to manage your own expectations for a disorder that has no clear course. This can cause enormous stress in parents who are often teetering between hope and setbacks.
To normalize DiGeorge syndrome in your life, start by educating yourself by working closely with your medical team and seeking quality medical information in clear and easy-to-understand language.19
A good place to start is by reaching out to the non-profits agencies like the International 22q11.2 Foundation in Matawan, New Jersey, or the 22q Family Foundation in Apto, California. In addition to providing practical advice, both organizations can refer you to local or online support groups of parents, families, and individuals living with DiGeorge syndrome
There is even a growing number of specialty clinics dedicated to children with DiGeorge syndrome.20
They include the 22q Clinic at Phoenix Children's Hospital, the 22q Deletion Clinic at the SickKids Hospital in Toronto, and the 22q Children's Clinic at Massachusetts General Hospital in Boston.
 Ebola Outbreak 2021 in Africa: Origin, Causes and Treatment of Disease Ebola Outbreak 2021 in Africa: Origin, Causes and Treatment of Disease For more than a year the world has been in turmoil because of the covid epidemic, now the Ebola outbreak in Africa continues to threaten ... |
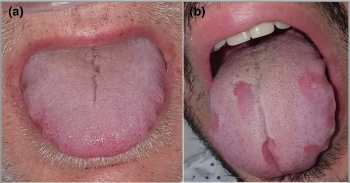 Facts about COVID Tongue: Peculiar virus Symptoms, Signs of Infection Facts about COVID Tongue: Peculiar virus Symptoms, Signs of Infection Facts about COVID Tongue: Is a swollen tongue or bumpy tongue a symptom of COVID-19? This COVID symptom is a serious mouthful? |
 What is LEPTOSPIROSIS: Symptoms, Causes, Transmission, Treatments for a Common Disease in India What is LEPTOSPIROSIS: Symptoms, Causes, Transmission, Treatments for a Common Disease in India Facts about LEPTOSPIROSIS, without timely treatment, can lead to kidney damage, meningitis (inflammation of the membrane around the brain and spinal cord), liver failure, respiratory ... |
 What are Influenza A and B Causes, Symptoms and Prevention What are Influenza A and B Causes, Symptoms and Prevention Flu is a contagious respiratory illness that can infect the nose, throat, and sometimes the lungs. Its symptoms can be mild or severe. The "flu" ... |
 What is Gonorrhoea: Symptoms, Causes and Prevention for most common disease in India What is Gonorrhoea: Symptoms, Causes and Prevention for most common disease in India Gonorrhea is a disease that is transmitted through sexual intercourse or baby vaginal delivery. Both men and women can get it, though men get ... |