What is LEPTOSPIROSIS: Symptoms, Causes, Transmission, Treatments for a Common Disease in India
 |
| Leptospirosis is a bacterial zoonosis that is common worldwide. Photo: Love You Doctor |
What is Leptospirosis
Leptospirosis is a bacterial zoonosis that is common worldwide, especially in developing countries. Organisms are shed in the urine of infected animals, including rodents and domesticated animals, which may not show signs of disease. Humans usually become ill after contact with infected urine, or through contact with water, soil, or food that has been contaminated. Outbreaks have been associated with floodwaters.
In animals, the clinical signs of leptospirosis are often related to kidney disease, liver disease, or reproductive dysfunction. In humans, many cases are mild or asymptomatic and go unrecognized. In some patients, however, the illness may progress to kidney or liver failure, aseptic meningitis, life-threatening pulmonary hemorrhage, and other syndromes.
Signs and Symptoms of Leptospirosis
In humans, Leptospirosis can cause a wide range of symptoms, including:
- High fever
- Headache
- Chills
- Muscle aches
- Vomiting
- Jaundice (yellow skin and eyes)
- Red eyes
- Abdominal pain
- Diarrhea
- Rash
According to World Health Organisation, in the early stages of the disease, symptoms include high fever, severe headache, muscle pain, chills, redness of the eyes, abdominal pain, jaundice, hemorrhages in the skin and mucous membranes, vomiting, diarrhea, and rash.
Many of these symptoms can be mistaken for other diseases. In addition, some infected persons may have no symptoms at all, CDC cites.
 |
| Symptoms of Leptospirosis. Photo: Medlife |
The time between a person’s exposure to a contaminated source and becoming sick is 2 days to 4 weeks. The illness usually begins abruptly with fever and other symptoms. Leptospirosis may occur in two phases:
- After the first phase (with fever, chills, headache, muscle aches, vomiting, or diarrhea) the patient may recover for a time but become ill again.
- If a second phase occurs, it is more severe; the person may have kidney or liver failure or meningitis.
The illness lasts from a few days to 3 weeks or longer. Without treatment, recovery may take several months.
Causes of Leptospirosis
Leptospirosis is caused by a bacterium called Leptospira interrogans. The organism is carried by many animals and lives in their kidneys. It ends up in soil and water through their urine.
If you’re around soil or water where an infected animal has peed, the germ can invade your body through breaks in your skin, like scratches, open wounds, or dry areas. It can also enter through your nose, mouth, or genitals. It’s hard to get it from another human, though it can be passed through sex or breastfeeding, as cited by WebMD.
 |
| Photo: Medlactec |
You’re at risk if you spend a lot of time around animals or in the outdoors. You’re more likely to be exposed to it if you have one of these jobs:
- Farmer
- Veterinarian
- Underground worker (you work in a sewer or a mine)
- Slaughterhouse worker
- Military personnel
Also, if you raft, swim, or camp near affected lakes and rivers, you could get the disease.
Leptospirosis is more often found in warm climates. And although the bacteria live all over the world, it’s especially common in Australia, Africa, Southeast Asia, Central and South America, and the Caribbean.
Transmission of Leptospirosis
Leptospirosis can be transmitted either directly between hosts or indirectly through the environment. Leptospira spp. can be ingested in contaminated food or water, spread in aerosolized urine or water, or transmitted by direct contact with the skin. The organisms usually enter the body through mucous membranes or abraded skin. They might also be able to penetrate intact skin that has been immersed for a long time in the water, although this is controversial.
Leptospira spp. are excreted in the urine of both acutely and chronically infected animals. Chronic carriers may shed these organisms for months or years. Although humans can also shed Leptospira in the urine, prolonged shedding seems to be uncommon; most people excrete these bacteria for 60 days or less. In animals, Leptospira can be found in aborted or stillborn fetuses, as well as in normal fetuses or vaginal discharges after giving birth. They can be isolated from the male and female reproductive organs in some species, and these infections may persist for long periods. For example, serovar Hardjo may be found in the reproductive tract of both cows and bulls for more than a year. In rare instances, human cases have also been transmitted during sexual intercourse, or by breastfeeding. Other uncommon routes of exposure in people include rodent bites and laboratory accidents, as cited by The Center for Food Security & Public Health.
Pathogenic Leptospira spp. do not multiply outside the host. In the environment, they require high humidity for survival and are killed by dehydration or temperatures greater than 50°C (122°F). These organisms may remain viable in the environment for several months under optimal conditions, e.g., in water or contaminated soil. They survive best in bodies of water that are slow-moving or stagnant.
Leptospirosis Treatment
According to The Center for Food Security & Public Health, various antibiotics including tetracyclines (e.g., doxycycline), penicillins, dihydrostreptomycin, and streptomycin may be used to treat leptospirosis. Fluid therapy, blood transfusions, respiratory support, and other supportive care may also be necessary.
The primary treatment for equine recurrent uveitis in horses is anti-inflammatory drugs and medications to decrease discomfort (e.g., mydriatic cycloplegics such as topical atropine). Surgery (pars plana vitrectomy) and other therapies may also be used.
 |
| Photo: Medical News Today |
Leptospirosis Prevention
Several human vaccines have been developed; all are serovar specific, developed for specific epidemiologic circumstances. None is widely available. Prevention measures include avoiding potential sources of infection, administration of prophylaxis for individuals at high risk of exposure, and animal vaccination.
The most important control measures for preventing human leptospirosis include avoiding potential sources of infection such as stagnant water and animal farm water runoff, rodent control, and protection of food from animal contamination.
Antimicrobial prophylaxis for individuals at high risk of exposure may be useful in some settings. Among more than 700 individuals in the Andaman Islands (a highly endemic setting in Southeast Asia where outbreaks of leptospirosis related to flooding are common) randomized to prophylaxis with weekly doxycycline or placebo, clinical infection rates were lower among those who received doxycycline (3.1 versus 6.8 percent), although there was no difference in seroconversion rates. In another study including more than 900 soldiers deployed for jungle training in Panama, fewer cases of leptospirosis were observed among those who received doxycycline prophylaxis (200 mg orally every week for two to three weeks and at the end of exposure) compared with placebo (1 versus 20 cases), reported UpToDate.
Vaccination of domestic and farm animals against leptospirosis can provide variable levels of protection. Some immunized animals become infected and excrete leptospires in their urine.
| Leptospirosis is now emerging in India as an important public health problem. Leptospirosis is endemic in 5 states & 1 union territory of India. The endemic states are Gujarat, Maharashtra, Kerala, Tamilnadu, Karnataka & the union territory of Andaman & Nicobar Islands. Gujarat reported 392 cases in 2005 with 81 deaths (mortality: 20.6%). Maharashtra reported 2355 cases in 2005 with 167 deaths. In Kerala, Kolenchery reported 976 cases with a mortality of 5.3%. Calicut reported 282 cases with a mortality of 6%. Seroprevalence in Calicut was 38.1% in high risk groups. 900 cases were treated in Kottayam over a period of 10 years. Leptospirosis is an important cause of acute febrile illness contributing to 16.8% following malaria which was 27%. Co-infection of leptospirosis with malaria occurred in 22% of cases. At present, Andaman Islands has probably the highest incidence rates of leptospirosis in India with figures ranging from 50 -65 cases / 100,000 per year. Leptospirosis is also considered to be the most widespread zoonotic disease in the world. According to the CDC, it’s estimated that more than 1 million cases occur worldwide each year, including about 59,000 deaths. |
If you find the aforementioned information effective and useful, don't hesitate to share it widely, many thanks in advance from Knowinsiders!
 What is Gonorrhoea: Symptoms, Causes and Prevention for most common disease in India What is Gonorrhoea: Symptoms, Causes and Prevention for most common disease in India Gonorrhea is a disease that is transmitted through sexual intercourse or baby vaginal delivery. Both men and women can get it, though men get ... |
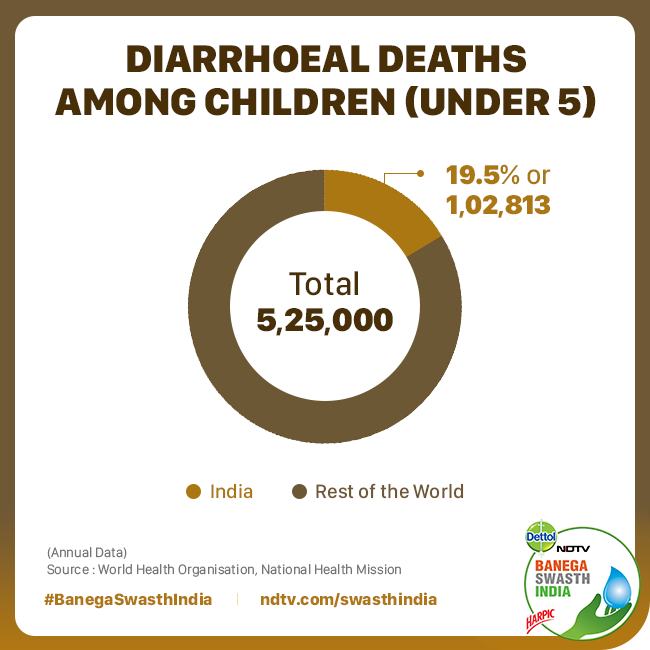 Diarrhea disease: Causes, Symptoms & Treatments for most common disease in India Diarrhea disease: Causes, Symptoms & Treatments for most common disease in India Diarrhoeal disease is the second leading cause of death in children under five years old and is responsible for killing around 525 000 children ... |
 Typhoid Fever: Symptoms, Causes, Transmission & Treatment for most common disease in India Typhoid Fever: Symptoms, Causes, Transmission & Treatment for most common disease in India Be careful since spring time is perfect for bacteria to cause some certain fevers, which include typhoid. Below Knowinsiders would give you critical knowledge about ... |