Jaundice: Symptoms, Causes, Transmission, Treatments for a Common Diseases in India
 |
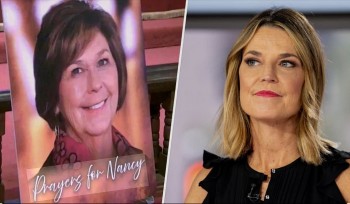
| Normal person and Jaundice patient. Photo: blog.houseofdiagnostics.com |
Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary tract obstruction. The prevalence of jaundice in adults is rare, while jaundice in babies is common with an estimated 80% affected during their first week of life. The most commonly associated symptoms of jaundice are itchiness, pale feces, and dark urine.
Normal levels of bilirubin in blood are below 1.0 mg/dl (17 µmol/l), while levels over 2–3 mg/dl (34-51 µmol/l) typically result in jaundice. High blood bilirubin is divided into two types - unconjugated bilirubin and conjugated bilirubin.
Types of Jaundice
Jaundice happens when too much bilirubin builds up in your blood. This makes your skin and the whites of your eyes look strikingly yellowish.
Bilirubin is a yellowish pigment created as hemoglobin — a component of red blood cells — is broken down.
Normally, bilirubin is delivered from the bloodstream into your liver. Then, it passes through tubes called bile ducts. These ducts carry a substance called bile into your small intestine. Eventually, bilirubin is passed out of your body through urine or stool.
Types of jaundice are categorized by where they happen within the liver’s process of taking in and filtering out bilirubin:
pre-hepatic: before the liver
hepatic: in the liver
post-hepatic: after the liver
Causes of Jaundice
Pre-hepatic
Jaundice in these cases is caused by a rapid increase in the breakdown and destruction of the red blood cells (hemolysis), overwhelming the liver's ability to adequately remove the increased levels of bilirubin from the blood, according to emedicinehealth.
Examples of conditions with increased breakdown of red blood cells include:
malaria,
sickle cell crisis,
spherocytosis,
thalassemia,
glucose-6-phosphate dehydrogenase deficiency (G6PD),
drugs or other toxins, and
autoimmune disorders.
Hepatic
Jaundice in these cases is caused by the liver's inability to properly metabolize and excrete bilirubin. Examples include:
hepatitis (commonly viral or alcohol-related),
cirrhosis,
drugs or other toxins,
Crigler-Najjar syndrome,
Gilbert's syndrome, and
cancer.
Post-hepatic
Jaundice in these cases, also termed obstructive jaundice, is caused by conditions that interrupt the normal drainage of conjugated bilirubin in the form of bile from the liver into the intestines.
Causes of obstructive jaundice include:
gallstones in the bile ducts,
cancer (pancreatic and gallbladder/bile duct carcinoma),
strictures of the bile ducts,
cholangitis,
congenital malformations,
pancreatitis,
parasites,
pregnancy, and
newborn jaundice.
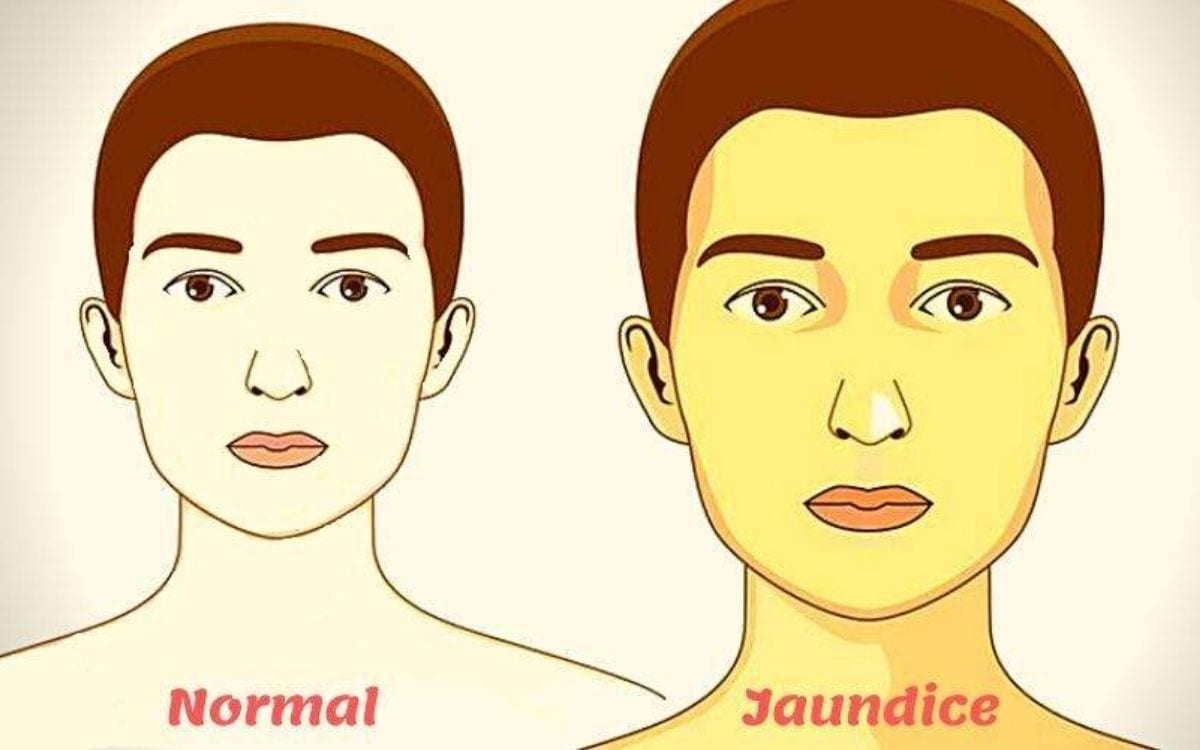
Jaundice Signs and Symptoms
 |
| Photo: blog.houseofdiagnostics.com |
The most common signs of jaundice in adults are a yellowish discoloration of the white area of the eye (sclera) and skin with scleral icterus presence indicating serum bilirubin of at least 3 mg/dl. Other common signs include dark urine (bilirubinuria) and pale,(acholia) fatty stool (steatorrhea). Because bilirubin is a skin irritant, jaundice is commonly associated with severe itchiness.
A much less common sign of jaundice specifically during childhood is yellowish or greenish teeth. In developing children, hyperbilirubinemia may cause a yellow or green discoloration of teeth due to bilirubin deposition during the process of tooth calcification. While this may occur in children with hyperbilirubinemia, tooth discoloration due to hyperbilirubinemia is not observed in individuals with adult-onset liver disease. Disorders associated with a rise in serum levels of conjugated bilirubin during early development can also cause dental hypoplasia.
Risk factors
Risk factors associated with high serum bilirubin levels include male gender, white ethnicities, and active smoking. Mean serum total bilirubin levels in adults were found to be higher in men (0.72 ± 0.004 mg/dL) than women (0.52 ± 0.003 mg/dL). Higher bilirubin levels in adults are found also in non-Hispanic white population (0.63 ± 0.004 mg/dL) and Mexican American population (0.61 ± 0.005 mg/dL) while lower in non-Hispanic black population (0.55 ± 0.005 mg/dL). Bilirubin levels are higher in active smokers.
Jaundice Diagnosis and Tests
According to medicalnewstoday, Doctors diagnose jaundice by checking for signs of liver disease such as:
Bruising of the skin.
Spider angiomas (abnormal collection of blood vessels near the surface of the skin).
Palmar erythema (red coloration of the palms and fingertips).
Urinalysis (urine testing) that's positive for bilirubin shows that the patient has conjugated jaundice. The findings of urinalysis should be confirmed by serum testing. The serum testing will include a complete blood count (CBC) and bilirubin levels.
Your doctor will also do an exam to determine the size and tenderness of your liver. He or she may use imaging (ultrasonography and computer tomographic (CT) scanning) and liver biopsy (taking a sample of the liver) to further confirm the diagnosis.
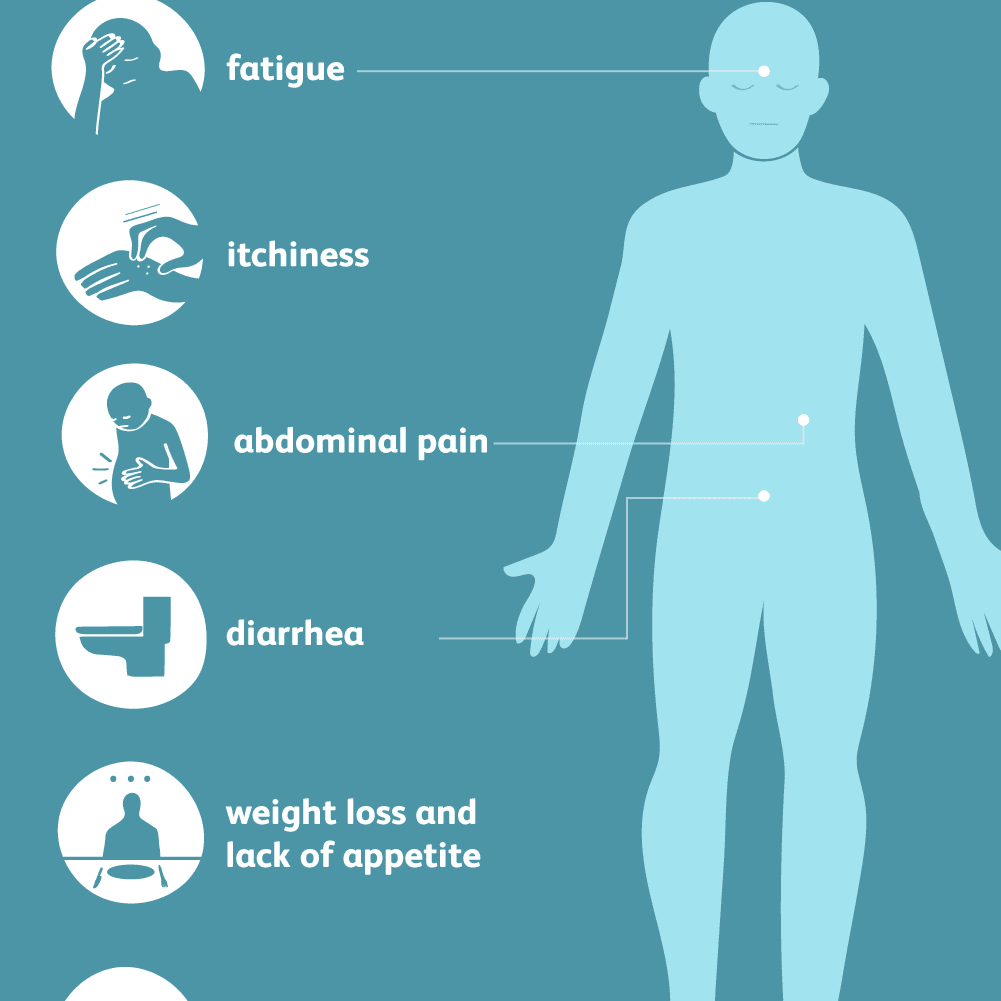
Jaundice Treatments
 |
| Jaundice treatment in baby. Photo: verywellfamily.com |
There's no treatment for jaundice as such, but the disease can be managed by managing symptoms and causes of jaundice, reported NHP India.
Pre-hepatic jaundice
In treating pre-hepatic jaundice, the objective is to prevent the rapid breakdown of red blood cells that's causing the level of bilirubin to build up in the blood.
In cases of infections, such as malaria, the use of medication to treat the underlying infection is usually recommended. For genetic blood disorders, such as sickle cell anemia or thalassemia, blood transfusions may be required to replace the red blood cells.
Gilbert's syndrome doesn't usually require treatment because jaundice associated with the condition isn't particularly serious and doesn't pose a serious threat to health.
Intra-hepatic jaundice
In cases of intra-hepatic jaundice, there's little that can be done to repair any liver damage, although the liver can often repair itself over time. Therefore, the aim of treatment is to prevent any further liver damage from occurring.
For liver damage that's caused by infection, such as viral hepatitis or glandular fever, anti-viral medications may be used to help prevent further damage.
If the damage is due to exposure to harmful substances, such as alcohol or chemicals, avoiding any further exposure to the substance is recommended.
In severe cases of liver disease, a liver transplant is another possible option.
Post-Hepatic Jaundice
In most cases of post-hepatic jaundice, surgery is recommended to unblock the bile duct system.
During surgery, it might be required to remove:
- The gallbladder
- A section of the bile duct system
- A section of the pancreas to prevent further blockages from occurring
NHP provides indicative information for a better understanding of health. For any diagnosis and treatment purpose consult a physician.
Jaundice Prevention
It's not possible to prevent all cases of jaundice because it can be caused by a wide range of conditions or circumstances.
However, by taking certain precautions the risk of developing jaundice can be minimized. These include:
- Ensuring not to exceed the recommended daily amount (RDA) for alcohol consumption.
- Maintaining a healthy weight for height and build.
- Vaccination against hepatitis A and hepatitis B.
- Avoid high-risk behaviors such as intravenous drug use or unprotected intercourse.
- Avoid potentially contaminated food/water and maintain good hygiene
- Avoid medications and toxins which can cause hemolysis or directly damage the liver.
Jaundice in IndiaIn the study of Doctors in Department of Pediatrics, ASRAM Medical College, Eluru, AP, India, out of 560 newborns delivered during the study period at ASRAM, 273 (48.8%) newborns developed clinical jaundice. Out of 273 newborns with clinical jaundice, 166 (61%) newborns developed physiological jaundice. The overall incidence of non-physiological jaundice in the study group is 19%. (107 out of 560 newborns ). Out of 273 newborns with clinical jaundice, 107 newborns developed pathological jaundice. Out of 107 newborns,52 (48%) newborns had breastfeeding jaundice.17 (16%) newborns had ABO incompatibility. 8 (7.54%) newborns were preterms. 6 (5.7%) newborns had cephalohematoma. 6 (5.7%) newborns had Rh incompatibility. 5 (4.8%) newborns had a history of previous sibling deaths. 4 (3.8%) newborns had a history of birth asphyxia. 4 (3.8%) newborns were born to mothers with a history of GDM.3 (2.8%) newborns had sepsis. 1 (0.93%) newborn was born to a mother with a history of hypothyroidism. 1 (0.93%) newborn was born to a mother with TORCH infection. Sex factor had an influence on the incidence of non-physiological jaundice among the neonates showing that males 67% (72 out of 107) had a higher incidence compared to females 33% (35 out of 107) with p-value <0.05. All 4 (100%) newborns with a history of birth asphyxia developed pathological jaundice. Out of 107 babies with pathological jaundice, 5 newborns had Rh incompatibility, 17 newborns had ABO incompatibility,1 newborn had both Rh and ABO incompatibility. Out of 273 newborns with clinical jaundice, 2 (1%) newborns required double volume exchange transfusion as a therapeutic intervention for the treatment of jaundice. Both these cases were associated with Rh incompatibility as a risk factor for pathological jaundice. |
 Top 10 Most Common Diseases in India Top 10 Most Common Diseases in India Despite being the 5th largest economy in the world, some areas of India still face with shortage of purified water, poverty and other necessities that ... |
 Hookworm Infection: Symptoms, Causes, Transmission, Treatments for a Common Diseases in India Hookworm Infection: Symptoms, Causes, Transmission, Treatments for a Common Diseases in India Hookworm infection is an infection of the intestines that can cause an itchy rash, respiratory and gastrointestinal problems, and eventually iron deficiency anemia due to ... |
 Filariasis: Symptoms, Causes, Transmission, Treatments of a Common Diseases in India Filariasis: Symptoms, Causes, Transmission, Treatments of a Common Diseases in India Filariasis is caused by several round, coiled and thread-like parasitic worms that belong to the family filaria. These parasites penetrate the skin either on their ... |