14 Most Common Andrological Diseases That Every Man Should Know
 |
| Most Common Andrological Diseases |
Common male diseases such as infertility, prostatitis, balanitis, cystitis, erectile dysfunction, etc. will be discussed in detail below by andrologists.
What is Andrology?
The term ‘andrology’ comes from the Greek word ‘Andros’, which means male. As its name implies, the field of andrology focuses on helping men with a number of male-related medical issues.
Disorders of the male reproductive system such as reduced male fertility or disorders of the male hormone production (amongst others testostoron) and/or sexual function.
The term andrology was formed by the combination of the Latin words andros (male) and logos (science) and its literal meaning means male science. Today, andrology is a branch of science that includes all clinical anatomical, physiological, and biochemical developments and surgery related to male and female sexual health, male infertility.
Top Most Common Andrological Diseases
1.Impotence
 |
| Andrology is a branch of medicine that examines the sexual health of men and women and many sexual diseases. |
Inability to have sexual intercourse, as a result of absent erections, but also as a result of an erection that is not firm enough or not firm for long enough.
Causes
- Reduced blood supply
- Constriction of the blood vessels leading to the penis, e.g. as a result of arteriosclerosis.
- Leakage of too much blood from the corpora cavernosa.
- Reduced innervation, as in diabetes patients and after surgery in the small pelvis:
- Prostate surgery
- Bowel surgery
- Hormonal causes: reduced libido ("desire") can lead to erectile dysfunction.
- Psychological causes (e.g. relational problems, performance anxiety, problems at work, ...)
Risk factors
- Smoking
- Obesity
- Diabetes
- High blood pressure
- High cholesterol
- Insufficient exercise
Treatment
Below you will find a number of possible treatment for this disorder. After the diagnosis your physician will, in consultation with you and the other physician of the team, choose the best solution for you. Your treatment can therefore differ from the therapy/ies suggested below.
- Medication
- Support from a sexologist or urologist in case of bij psychiatric or relational problems.
- Intracavernous injections (e.g. with papaverine) to stimulate erections, in case of problems with innervation.
- Implantation of a penile or erectile prosthesis
2.Reduced male fertility
Causes
Fertility problems in men are often related to deviations in the sperm cells. These can be caused by disorders in:
-Sperm production
-Sperm transport
-Hormones that stimulate sperm production
It is however important to be aware that in at least half the cases there is no proper medical explanation for reduced male fertility.
Sperm production
Problems in sperm production can lead to reduced sperm count, reduced motility or sperm shape abnormalities.
Numerous factors can be at the base:
- Infection or inflammation of the testes (e.g. mumps virus or STDs such as gonorrhea)
- Varicocele (testicular varicose vein)
- Scar tissue after injury or damage to the scrotum and testes
- Torsion of the testes, cutting off the blood supply to the testes
- Undescended testes or other deviating positions
- Genetic disorders
- Damaged separation between the seminal ducts and blood vessels
- Medication that reduce fertility (sometimes temporarily) (e.g. anabolics)
- Chemotherapy and radiation
- Pesticides and chemical substances
Sperm transport
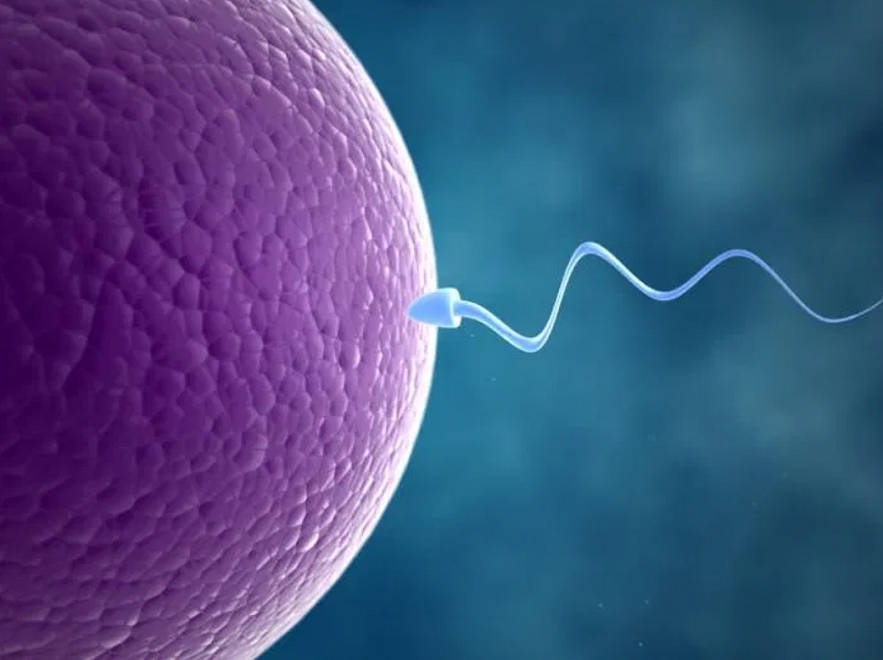
Even if the sperm is of good quality, it still needs to reach the egg cell. A disorder in sperm transportation is another cause of reduced male fertility.
Potential reasons for a transportation disorder:
- Erectile dysfunctions, where the penis is not firm enough, or not firm for long enough, to have normal sexual intercourse.
- Premature ejaculation, where the semen is not ejected deep enough in the vagina.
- Retrograde ejaculation, where semen flows back to the man's bladder.
- Obstruction of the ejaculatory ducts, which leads to a lack of sperm in the ejaculate (e.g. in case of cystic fibrosis or after vasectomy).
Hormones stimulating sperm production
Sometimes the body does not produce sufficient hormones that stimulate sperm production.
Such a disorder can also lead to reduced male fertility.
Treatment
Below you will find a number of potential treatments for this disorder. After the diagnosis, your doctor will, in consultation with you and the other doctors of the team, choose the best solution for you. Your treatment can therefore deviate from the therapy or therapies proposed below.
3.Premature Ejaculation
This is a common disease in men with the manifestation that the patient is almost unable to control ejaculation, leading to feelings of discomfort, boredom in relationships and affecting marital life.
However, the disease is curable if treated early. Premature ejaculation due to psychological factors can be overcome by itself, but if the condition persists, it should be diagnosed and treated by a specialist, absolutely should not take drugs arbitrarily.
In the U.S., about 1 in 3 men 18 to 59 years old have problems with PE. The problem is often thought to be psychological, but biology may also play a role.
Causes
Serotonin
Though the exact cause of PE is not known, serotonin may play a role. Serotonin is a natural substance in your body made by nerves. High amounts of serotonin in the brain increase the time to ejaculation. Low amounts can shorten the time to ejaculation, and lead to PE.
Psychological Issues
Psychological, or mental health, issues can be involved in PE and may include:
- depression
- stress
- guilt
- unrealistic expectations about sexual performance
- history of sexual repression
- lack of confidence
- relationship problems
Taking care of emotional problems often helps.
Other Issues
PE and Age
PE can happen at any age. Aging is not a direct cause of PE, though aging does cause changes in erections and ejaculation. For older men, erections may not be as firm or as large. Erections may not last as long before ejaculation occurs. The feeling that ejaculation is about to happen may be shorter. These changes can lead to an older man ejaculating earlier.
PE and Your Partner
With PE, you may feel you lose some of the closeness shared with a sexual partner. You might feel angry, ashamed or upset, and turn away from your partner. Premature ejaculation may not only affect you, it may also affects your partner. PE can cause partners to feel less connected or feel hurt.
Talking about the problem is an important step. Couples counseling or sex therapy can be helpful. Exercises, such as the squeeze technique, may be helpful for you and your partner to prolong an erection (see the treatment section of this article for details). Most importantly, a couple should learn ways to relax. Worry (such as performance anxiety) can make PE worse.
Diagnosis
It is typical for men to be able to have at least some control of if and when they ejaculate during partnered sex and masturbation. If a man does not feel that he has control of when ejaculation occurs, and if there is worry by the man or his sexual partner(s), PE may be present.
When PE gets in the way of your sexual pleasure, you should see your health care provider. The diagnosis is determined by whether ejaculation occurs early, late, or not at all. Most often, your health care provider will diagnose PE after a physical exam and talking with you. Some questions he or she may ask are:
- How often does PE happen?
- How long have you had this problem?
- Does this happen with just one partner, or all partners?
- Does PE happen with each attempt at sex?
- What type of sexual activity (i.e., foreplay, masturbation, intercourse, use of visual cues, etc.) do you take part in and how often?
- How has PE changed your sexual activity?
- How are your personal relationships?
- Is there anything that makes PE worse or better (i.e., drugs, alcohol, etc.)?
Lab testing is only needed if your health care provider finds something during your physical exam.
Treatment
Psychological therapy, behavioral therapy and drugs are the main treatments for PE. You can talk with your health care provider to decide the best choice for you. More than one type of treatment may be used at the same time.
Psychological Therapy
Psychological therapy is a way to work through the feelings and emotions that may lead to problems with sexual relationships. The goal of this type of therapy is to learn the source of problems and find solutions that may help PE. It can also help couples learn to grow closer. Psychological therapy can help you become less nervous about sexual performance. It can also give you greater sexual confidence and understanding to help your partner's satisfaction. This type of therapy can be used as the only treatment, or it may be used along with medical or behavioral therapy.
Behavioral Therapy
Behavioral therapy uses exercises to help build tolerance to delay ejaculation. The goal is to help you train your body away from PE. Some choices are the squeeze method and the stop-start method. Exercises work well, but they may not be a lasting answer.
The Squeeze Method
With this method, you or your partner stimulates your penis until you are close to ejaculation. When you are close, you or your partner firmly squeezes your penis so your erection partly goes away. The goal is for you to become aware of the sensations leading to climax. The squeeze method may help you better control and delay climax on your own
The Stop-Start Method
In this method, you or your partner stimulates your penis until just before ejaculation. When you are about to climax, you or your partner stops until the urge to climax lets up. As you regain control, you and your partner start stimulating your penis again. This process is repeated 3 times. You ejaculate on the fourth time. You repeat this method 3 times a week until you have gained more control.
Medical Therapy
No drugs have been approved in the U.S. to treat PE. Still, there are a number of drugs, numbing creams and numbing sprays that may slow ejaculation in men with PE.
Drugs
Doctors noticed that men and women on antidepressants have delayed orgasms. Drugs such as fluoxetine, paroxetine, sertraline, clomipramine and tramadol affect serotonin levels. Some doctors use these drugs "off-label" (for a different reason than the drug's original use) to treat PE. If one drug does not work, your doctor may suggest you try a different drug.
For others, α1-Adrenoceptor antagonists are another option for drug therapy. These drugs may induce ejaculatory dysfunction such as retrograde ejaculation and/or failure of emission.
Drugs for PE can be taken each day or only before sex. Your health care provider will suggest when you should take a drug based on your activity level. The best time to take the drug is not clear. Most doctors suggest from 2 to 6 hours before sex. PE can return if you stop taking these drugs. Most men with PE need to take these drugs on an ongoing basis.
Numbing Creams or Sprays
Numbing creams and sprays may be put on the head of the penis about 20 to 30 minutes before sex. If you leave the numbing cream/spray on your penis for longer than suggested, your erection may go away. Also, the numbing cream/spray should not be left on the exposed penis during vaginal sex because it may cause vaginal numbness. Wash the cream off your penis 5 to 10 minutes before sex. Wearing a condom can also help dull sensation.
After Treatment
With the techniques listed here, about 95 out of 100 men will recover from PE. There is no way to promise recovery, but learning how to relax may help. If the problem stays, keep working with your health care provider to find solutions.
| Premature Ejaculation and Erectile Dysfunction (ED) Sometimes PE is a problem for men who have erection problems (erectile dysfunction or ED). This is when men are not able to get or keep an erection that's firm enough for sex. Since an erection goes away after ejaculation, it can be tough to know if the problem is PE or ED. ED should be treated first. Premature ejaculation may not be a problem once the ED is treated |
4.Infertility in Men
 |
| Infertility in Men |
Infertility is a condition in which couples live together and have regular unprotected intercourse for 1 year but still do not have children. Infertility disease is also quite common in today's society, with causes that can come from both husband and wife. The main preventive measure is to go to the reproductive health periodically to detect it early and increase the effectiveness of treatment.
In the United States, around 10 percentTrusted Source of women aged 15 to 44 years are estimated to have difficulty conceiving or staying pregnant. Worldwide, 8 to 12 percentTrusted Source of couples experience fertility problems. Between 45 and 50 percent Trusted Sourceof cases are thought to stem from factors that affect the man.
The following are common causes of infertility in men:
Semen and sperm
Share on Pinterest Sometimes the sperm cannot travel effectively to meet the egg.
Semen is the milky fluid that a man’s penis releases during orgasm. Semen consists of fluid and sperm. The fluid comes from the prostate gland, the seminal vesicle, and other sex glands.
The sperm is produced in the testicles.
When a man ejaculates and releases semen through the penis, the seminal fluid, or semen, helps transport the sperm toward the egg.
The following problems are possible:
- Low sperm count: The man ejaculates a low number of sperm. A sperm count of under 15 million is considered low. Around one third of couples have difficulty conceiving due to a low sperm count.
- Low sperm mobility (motility): The sperm cannot “swim” as well as they should to reach the egg.
- Abnormal sperm: The sperm may have an unusual shape, making it harder to move and fertilize an egg.
If the sperm do not have the right shape, or they cannot travel rapidly and accurately towards the egg, conception may be difficult. Up to 2 percentTrusted Source of men are thought to have suboptimal sperm.
Abnormal semen may not be able to carry the sperm effectively.
This can result from:
- A medical condition: This could be a testicular infection, cancer, or surgery.
- Overheated testicles: Causes include an undescended testicle, a varicocele, or varicose vein in the scrotum, the use of saunas or hot tubs, wearing tight clothes, and working in hot environments.
- Ejaculation disorders: If the ejaculatory ducts are blocked, semen may be ejaculated into the bladder
- Hormonal imbalance: Hypogonadism, for example, can lead to a testosterone deficiency.
Other causes may include:
- Genetic factors: A man should have an X and Y chromosome. If he has two X chromosomes and one Y chromosome, as in Klinefelter’s syndrome, the testicles will develop abnormally and there will be low testosterone and a low sperm count or no sperm.
- Mumps: If this occurs after puberty, inflammation of the testicles may affect sperm production.
- Hypospadias: The urethral opening is under the penis, instead of its tip. This abnormality is usually surgically corrected in infancy. If the correction is not done, it may be harder for the sperm to get to the female’s cervix. Hypospadias affects about 1 in every 500 newborn boys.
- Cystic fibrosis: This is a chronic disease that results in the creation of a sticky mucus. This mucus mainly affects the lungs, but males may also have a missing or obstructed vas deferens. The vas deferens carries sperm from the epididymis to the ejaculatory duct and the urethra.
- Radiation therapy: This can impair sperm production. The severity usually depends on how near to the testicles the radiation was aimed.
- Some diseases: Conditions that are sometimes linked to lower fertility in males are anemia, Cushing’s syndrome, diabetes, and thyroid disease.
Some medications increase the risk of fertility problems in men.
- Sulfasalazine: This anti-inflammatory drug can significantly lower a man’s sperm count. It is often prescribed for Crohn’s disease or rheumatoid arthritis. Sperm count often returns to normal after stopping the medication.
- Anabolic steroids: Popular with bodybuilders and athletes, long-term use can seriously reduce sperm count and mobility.
- Chemotherapy: Some types may significantly reduce sperm count.
- Illegal drugs: Consumption of marijuana and cocaine can lower the sperm count.
- Age: Male fertility starts to fall after 40 years.
- Exposure to chemicals: Pesticides, for example, may increase the risk.
- Excess alcohol consumption: This may lower male fertility. Moderate alcohol consumption has not been shown to lower fertility in most men, but it may affect those who already have a low sperm count.
- Overweight or obesity: This may reduce the chance of conceiving.
- Mental stress: Stress can be a factor, especially if it leads to reduced sexual activity.
Laboratory studies have suggested that long-term acetaminophen use during pregnancy may affect fertilityTrusted Source in males by lowering testosterone production. Women are advised not to use the drug for more than one day.
Treatment
Treatment will depend on many factors, including the age of the person who wishes to conceive, how long the infertility has lasted, personal preferences, and their general state of health.
Frequency of intercourse
The couple may be advised to have sexual intercourse more often around the time of ovulation. Sperm can survive inside the female for up to 5 days, while an egg can be fertilized for up to 1 day after ovulation. In theory, it is possible to conceive on any of these 6 days that occur before and during ovulation.
However, a survey has suggested that the 3 days most likely to offer a fertile window are the 2 days before ovulation plus the 1 day of ovulation.
Some suggest that the number of times a couple has intercourse should be reduced to increase sperm supply, but this is unlikely to make a difference.
Fertility treatments for men
Treatment will depend on the underlying cause of the infertility.
- Erectile dysfunction or premature ejaculation: Medication, behavioral approaches, or both may help improve fertility.
- Varicocele: Surgically removing a varicose vein in the scrotum may help.
- Blockage of the ejaculatory duct: Sperm can be extracted directly from the testicles and injected into an egg in the laboratory.
- Retrograde ejaculation: Sperm can be taken directly from the bladder and injected into an egg in the laboratory.
- Surgery for epididymal blockage: A blocked epididymis can be surgically repaired. The epididymis is a coil-like structure in the testicles which helps store and transport sperm. If the epididymis is blocked, sperm may not be ejaculated properly.
5.CHH and Kallmann Syndrome
Congenital hypogonadotropic hypogonadism (CHH) is characterised by a deficiency of the gonadotropin releasing hormone (GnRH) in the brain. It is a genetic disorder which prevents spontaneaous puberty. Some men also have a problem with their sense of smell (Kallmann syndrome).
Symptoms
Congenital hypogonadotropic hypogonadism (CHH) is usually diagnosed when a child does not go into puberty.
Typical characteristics of congenital hypogonadotropic hypogonadism (CHH) are:
- In boys: small testicles, a small penis, undescended testicles, reduced beard growth and body hair, less muscle mass and a reduced libido
- In girls: no or little breast development
Additional symptom in Kallmann syndrome
A typicial additional sympom in case of the Kallmann syndrome:
- An impaired sense of smell
Causes
The cause of a congenital hypogonadotropic hypogonadism is an absent or distorted production of the gonadotropin releasing hormone (GnRH) in the brain. This will stop the brain from sending signals to the reproductive organs, stopping the production of sex hormones. This will halt puberty and cause infertility.
In addition to the impaired production of sex hormones, Kallmann syndrome also presents patients with a problem with the sense of smell (absent or strongly reduced), caused by the fact that the part of the brain that is used to smell has not been formed.
Treatments
The treatment consists of the administration of sex hormones.
- In men: testosterone
- In women: Progesterone and oestrogen
Fertility treatment may be required in case of a pregnancy wish.
Follow-up at the endocrinologist
The endocrinologist is best placed to coordinate the medical problems related to congenital hypogonadotropic hypogonadism and Kallmann syndrome, and if necessary to refer to other specialists concerned (fertility specialist ... ).
6.Gynaecomastia
Development of abnormal breast tissue in boys and men. Excessive mammary gland development can lead to pain and aesthetic suffering in men.
Causes
At birth both boys and girls have little glandular ducts behind the nipple. In boys these usually disappear during childhood.
During puberty these mammary glands can start to swell (temporarily). In case of gynaecomastia there is excessive mammary gland development.
Causes of gynaecomastia in men:
- Imbalance between male and female sex hormones
- Liver disorder
- Testicular disorder
Treatment
Below you will find a number of possible treatment for this disorder. After the diagnosis your physician will, in consultation with you and the other physician of the team, choose the best solution for you. Your treatment can therefore differ from the therapy/ies suggested below.
- Modify medication
- Antioestrogen for several months
- Plastic surgery (in case of persistent gynaecomastia primarily with aesthetic suffering)
7.Hypogonadism
A condition in which the testicles do not produce enough of the male hormone testosterone.
Cause
Hypogonadism can have several causes.
- Position of the testicles, disorders of the scrotum and other internal testicular disorders (primary hypogonadism)
- Lack of a signal from the brain (hypophysis) to the scrotum for the production of testosterone (secondary hypogonadism).
- Metabolic causes (e.g. obesity)
- Use of anabolic steroids
Consequences and symptoms
Possible effects and characteristics of a testosterone deficiency:
- Reduced fertility
- Increased fat mass
- Reduced muscle mass and bone density
- Stunted growth in children
- Absent or delayed puberty
- Loss of (muscle) strength
- Fatigue, anaemia and depression
- Fewer male characteristics (e.g. less or no body hair)
8.Klinefelter's Syndrome
Congenital chromosome condition in which men have two or more X-chromosomes (e.g. XXY or XXXY instead of XY). Nearly all men with the Klinefelter syndrome are infertile.
Additional X-chromosome
Normally, men have 1 X-chromosome and 1 Y-chromosome (XY). Men with the Klinefelter's syndrome have in addition to the Y-chromosome 2 or more X chromosomes (XXY, XXXY, …).
Cause
Klinefelter's is usually the result of a division error of the chromosomes in the reproductive cell of the mother or father.
For instance, a sperm cell will get both an X and a Y chromosome, or an egg cell both X's.
If a XY-sperm cell fertilises an egg cell, or if an XX egg cell merges with a sperm cell with a Y chromosome, it will result in the chromosome pattern 47, XXY.
Results
Nearly all men with Klinefelter's are infertile. At a young age it usually goes unnoticed.
The disorder is often diagnoses by accident, e.g. as a result of fertility problems.
Symptoms
The major symptoms of Klinefelter's syndrome are:
- Absence of sperm cells
- Infertility
- Impaired testicular development during puberty
- Delayed puberty or delayed sexual development
- Testosterone deficiency resulting in reduced development of male sex characteristics and reduced bone density
- Children with Klinefelter's syndrome are usually a little bit taller than their peers.
In some rare case we see delayed language and speech development or distorted motor development.
Risk factors and genetics
- Occurs only in men (sex chromosome disorder)
- Congenital, but not hereditary
Treatment
A testosterone treatment can be beneficial for the development of male sex characteristics and increased bone density. Possibilities for a fertility treatment will be examined in consultation with the fertility centre.
Tests and diagnosis
In case of this disorder, or if we suspect this disorder, we will perform one or several of the following examinations:
- Chromosome examination
- Blood test to determine the amount of testosterone
- Physical examination of the testicles and other sex characteristics
- Bone densitometry
- Klinefelter's syndrome can already be diagnosed during pregnancy based on a CVS test or an amniocentesis.
9.Erectile Dysfunction (ED)
 |
| Erectile dysfunction is a condition in which the penis is not able to get an erection or has an incomplete erection |
Erectile dysfunction is a condition in which the penis is not able to get an erection or the erection is incomplete, or the time is too short for sexual intercourse. This condition can lead to impotence. Although the disease is not too dangerous to health, it greatly affects the quality of family life, faith and bravery of men. If the disease is detected, it is necessary to go to the medical facilities immediately for diagnosis and appropriate treatment.
Approximately one in 10 adult males will suffer from ED on a long-term basis.
Many men do experience occasional failure to achieve erection, which can occur for a variety of reasons, such as drinking too much alcohol, stress, relationship problems, or from being extremely tired.
The failure to get an erection less than 20% of the time is not unusual and typically does not require treatment. However, the failure to achieve an erection more than 50% of the time generally means that there is a problem and treatment is needed.
ED does not have to be a part of getting older. While it is true that some older men may need more stimulation, they should still be able to achieve an erection and enjoy intercourse.
What causes erectile dysfunction (ED)?
ED can be caused by a number of factors, including:
- Vascular disease: Blood supply to the penis can become blocked or narrowed as a result of vascular disease such as atherosclerosis (hardening of the arteries).
- Neurological disorders (such as multiple sclerosis): Nerves that send impulses to the penis can become damaged from stroke, diabetes, or other causes.
- Psychological states: These include stress, depression, lack of stimulus from the brain and performance anxiety.
- Trauma: An injury could contribute to symptoms of ED.
Chronic illness, certain medications, and a condition called Peyronie's disease can also cause ED. Operations for the prostate, bladder, and colon cancer may also be contributing factors.
What doctors treat erectile dysfunction?
The type of medical specialist who treats ED will depend on the cause of the problem. Based on your family's medical history, as well as your own medical history and current health, your doctor may treat you with oral medications (Viagra®, Levitra®, Cialis®).
If these options fail, you may be referred to a urologist who can assist with other non-surgical options such as vacuum device or injections or surgical treatment options. If needed, your doctor may also refer you to a psychologist specializing in sexual dysfunction.
How is erectile dysfunction treated?
ED can be treated in many ways, including:
- Oral medications.
- Sex therapy.
- Penile injections.
- Vacuum devices.
- Intraurethral medication.
- Surgery (penile implant).
Each type has its own pros and cons. Discuss your options with your doctor to determine the best treatment for you.
The first step to treating ED is to find the underlying cause. Then the appropriate treatment can begin. There are a number of non-surgical and surgical options that can help a man regain normal sexual function.
10.Urethritis
Urethritis is an inflammatory disease that occurs in the urethral canal due to infectious causes that should be diagnosed and treated early to avoid complications such as cystitis, prostatitis or orchitis.
The main symptoms of urethritis include:
-Painful urination, burning urine, frequent urge to urinate;
-Pain along the urinary tract, yellow, cloudy or foul discharge in the urinary tract.
Urethritis is swelling and irritation or inflammation of the urethra. Urethritis is most commonly caused by bacteria or a virus, but can also result from physical injury or sensitivity to some chemicals in spermicides and contraceptive foams and jellies.
Symptoms of Urethritis
The primary symptoms of urethritis are urethral inflammation and painful urination. In addition, urethritis symptoms include:
- frequent or urgent need to urinate
- difficulty starting urination
- itching, pain or discomfort when not urinating
- pain during sex
- vaginal or urethral discharge
- abdominal and pelvic pain
- fever and chills
Diagnosing Urethritis
If you are experiencing painful urination or vaginal or urethral discharge, your doctor may assume an infection is present and may prescribe antibiotics immediately while awaiting test results. Tests can help confirm the diagnosis of urethritis and its cause and can include:
- physical examination of the genitals, abdomen and rectum to check for discharge and tenderness
- urine tests for gonorrhea, chlamydia or other bacteria
- examination of any discharge under a microscope
Blood tests are sometimes performed, but are not often necessary for an accurate diagnosis.
Treating Urethritis
The goal of any treatment for urethritis is to eliminate the cause of infection, prevent the spread of infection and improve your symptoms. There are different treatment options depending on the cause and severity of infection. Pain relievers may also be used in conjunction with other medications to lessen painful symptoms of urethritis .
People with urethritis who are being treated should avoid sex or use condoms during intercourse. If an infection is the cause of the inflammation, your sexual partner must also be treated.
Treating urethritis caused by bacteria
Antibiotics can successfully cure urethritis caused by bacteria. Many different antibiotics can treat urethritis, but some of the most commonly prescribed include:
- Doxycycline (Adoxa, Monodox, Oracea, Vibramycin)
- Ceftriaxone (Rocephin)
- Azithromycin (Zithromax, Zmax)
Urethritis due to trichomonas infection (called trichomoniasis) is usually treated with an antibiotic called Flagyl (metronidazole). Tindamax (tinidazole) is another antibiotic that can treat trichomoniasis. Urethritis that does not clear up after antibiotic treatment and lasts for at least six weeks is called chronic urethritis. Different antibiotics may be used to treat this problem.
Treating urethritis caused by a virus
Urethritis due to the herpes simplex virus can be treated with a number of medications, including:
- Famciclovir (Famvir)
- Valacyclovir (Valtrex)
- Acyclovir (Zovirax)
Preventing Urethritis
Urethritis can be prevented with good personal hygiene and by practicing safer sexual behaviors such as monogamy (one sexual partner only) and using condoms.
Urethritis is preventable and curable, but can lead to permanent damage to the urethra as well as other organs in women. Common complications from urethritis include:
-bladder infection (cystitis)
-cervicitis
-pelvic inflammatory disease (PID)
-urethral strictures
11.Inguinal Mushroom
This is a pathology in a rather hot and humid area of the body, which is an ideal environment for the fungus to grow. The disease usually occurs in summer with prolonged heat waves. Symptoms of the disease include:
Itching in the intimate area, groin area, inner thigh and spreading toward the buttocks or around the anus;
Lesions form patches with well-defined margins, scaly, and small papules around the margins. The affected area is usually dark in color and occurs in both groins.
The disease can be completely cured if diagnosed and treated early.
12.Prostatitis
The disease occurs mainly in adult men, causing many disturbances to daily activities and reducing quality of life. The main symptoms of this disease include:
Pain or discomfort in the perineum, testicles, abdomen, urethra, lower back, pelvis, anus, groin, penis;
Difficulty urinating, urinary frequency or urgency, pain when urinating, abnormal color of urine;
Sex life changes.
13.Phimosis
Foreskin stenosis is a narrowing of the foreskin at the end of the foreskin, making it impossible to completely pull the glans off the glans. This condition is mostly normal in infants and will go away as the child gets older. However, if a foreskin stenosis occurs and doesn't go away on its own, it can cause symptoms such as:
Difficulty urinating (straining, flushing when urinating) can affect kidney function if left untreated;
The foreskin is swollen and inflamed (swollen, hot, red, painful) with an unusual discharge or discharge.
14.Varicose veins of the testicles
This is a form of disease caused by blood stagnation in the venous system around the testicles for a long time, causing the veins to dilate, restricting blood supply to the testicles, causing damage to the function of the testicles.
The symptoms of testicular varices are often not obvious, mainly a feeling of heaviness, discomfort or pain in the testicles, especially when exercising too much or standing or sitting for a long time.
The prevalence of varicose veins in healthy young adults is about 15% and rises to 40% in infertile individuals. The disease does not exclude any age but occurs mainly in adult men.
When should you see an Andrologist?
Andrologists are largely urologists, or endocrinologists in some circumstances, at least in the UK. However, depending on the condition or procedure, a patient may see other types of specialists, including surgeons or psychiatrists. Andrology covers a wide number of conditions and functions, including male fertility, penile problems, and genitourinary disorders. Specialists in andrology may deal with procedures such as vasectomy, prostatectomy, and circumcision.
If you are having an issue with reproduction, hormone issues or your penis, you may be referred to an Andrologist. Andrologists are able to manage a range of conditions relating to men’s health. These include:
- Erectile dysfunction
- Male fertility issues
- Sexual dysfunction
- Prostate disease including prostatitis (inflammation of the prostate)
- Penile and testicular cancers
- Premature ejaculation.
What are some of the more common diagnostic tests in Andrology?
There are a range of tests that may be recommended by an Andrologist, or a specialist who manages reproductive health issues. These include:
Semen analysis
Semen is the name of the male reproductive fluid that contains spermatozoa (also known as ‘sperm’). A semen analysis is an andrology test that’s done to check on different parameters, including the:
- Volume and consistency of the semen
- Number of sperm present in the semen
- Ability of the sperm to move (known as their ‘motility’)
- Size and shape of sperm (known as their ‘morphology’).
A semen analysis is considered the most important andrology test for male infertility. In order to perform a semen analysis, you need to produce a semen sample (often referred to as a ‘sperm sample’). Providing this sample requires ejaculating directly into a clean specimen jar that your health practitioner will provide.
Semen samples need to be analysed soon after they are collected. That is why you will either need to bring your sample to your clinic soon after producing it, or collect the semen sample at a clinic in the first place. For more information about this andrology test, please talk to your doctor.
Sperm processing for Assisted Reproductive Technology (ART)
Before embarking on a reproductive therapy such as Assisted Reproductive Technology (ART), your fertility specialist will require a sperm sample. The sperm is collected in the same way as a semen analysis (see above). Once the semen has been collected, the scientist can process the sample.
Part of processing the semen involves separating the sperm from the surrounding seminal fluid. After the sperm has been separated, it is washed and examined. The sperm can then be used as part of a therapy to help conception, such as in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI).
Post-vasectomy semen analysis
After having a vasectomy, it’s important to have a semen analysis to check that your semen no longer contains sperm. Once your semen no longer contains sperm, you cannot impregnate a female partner. It takes some time after a vasectomy for semen to no longer contain sperm. That is why a post-vasectomy semen analysis should be performed at least three months after a vasectomy, or after at least 20 ejaculations.
If you are sexually active during that time, you should wear a condom to prevent pregnancy in a female partner. The post-vasectomy semen analysis should occur after you have abstained from ejaculating for at least 48 hours, but not longer than seven days. The sample is collected in the same way as a semen analysis (as per above). Once the test comes back showing there is ‘complete azoospermia’ (meaning no sperm were present in the sample collected), no further tests are needed.
Testicular biopsy evaluations
Your fertility specialist may organise a testicular biopsy to check whether there are issues with sperm production caused by a blockage. A testicular biopsy can also help determine the cause of other andrology issues, such as a lump in the testicles, or to diagnose testicular cancer. This andrology procedure is usually performed as an outpatient, either in your doctor’s rooms or at a hospital. Your doctor may recommend performing a testicular biopsy while you are awake, using anaesthesia and/or a sedative.
Alternatively, your doctor may recommend being asleep for the procedure (under a general anaesthetic). During the procedure, your doctor will make an incision and take a small sample of testicular tissue. The biopsy itself typically takes around 15 — 20 minutes. After this procedure, your doctor may advise refraining from sexual activity for one to two weeks.
Please talk to your specialist about any further concerns or questions relating to this procedure.
Conclusion
The Andrological diseases are a group of diseases belonging to the genitals of men that greatly affect health as well as sexual life. Current studies show that the proportion of men with Andrological Diseases is increasing. However, because it is a delicate issue, sufferers are often afraid to share and make the condition even more dangerous, affecting reproductive health and quality of marriage and family life.
Men who find themselves showing signs of any kind of male disease should see a doctor to most accurately diagnose the condition they are suffering from and take timely intervention measures, should not be subjective or afraid to visit.
 Top 15 Most Common Infectious Diseases in America (part 2) Top 15 Most Common Infectious Diseases in America (part 2) People in the United States continue to get diseases that are vaccine-preventable. |
 Top 15 Most Common Infectious Diseases in America (Part 1) Top 15 Most Common Infectious Diseases in America (Part 1) People in the United States continue to get diseases that are vaccine-preventable. The list below aims to provide basic information about the top 15 |